In Western countries, the rates of pancreatic cancer have increased significantly over the last few years. Pancreatic cancer is associated with a high mortality rate, and is the third leading cause of cancer-related death in the United States. In Europe and the United States, the incidence rate of new cases of pancreatic cancer is 7.7 per 100,000 people. In Greece, the incidence rate of new cases of pancreatic cancer is 9.2 for men and 5.6 for women. Overall, the incidence rate of new cases of pancreatic cancer is equal to 7.4 per 100,000 people annually. In other words, in Greece, 740 people are diagnosed with pancreatic cancer every year. Unfortunately, in about half of the patients, pancreatic cancer has already metastasized at the time of diagnosis, while in many other cases, pancreatic cancer is considered unresectable due to the size of the tumor. Pancreatic cancer is surgically resectable in no more than 15% of diagnosed patients.
The pancreas is surrounded by vital organs and is close to important arteries and veins of the abdomen. Pancreatic tumors often go undetected in the early stages as the symptoms they cause are often mistakenly attributed to “indigestion,” “gastritis,” gallstones, or even back pain. The surgery performed to remove the head of the pancreas, also known as the Whipple procedure, is the most technically demanding surgery and requires the highest level of expertise among all abdominal surgeries. It is by far the most complex and technically demanding procedure. The knowledge and experience needed to perform this procedure are hard to find. This is exactly why most surgeons consider over 95% of these tumors unresectable. Of course, some of these tumors may indeed be unresectable if, for instance, they have already metastasized at the time of the diagnosis. However, others are often considered unresectable simply because they are large or spread to the duodenum or major arteries and veins.
Our specialized and longstanding focus on pancreatic diseases (as easily seen in American and international medical literature) has helped us develop methods to successfully manage pancreatic tumors even when they are initially considered “unresectable.”
Some examples of our work are presented below:
1. Tumors that invade the portal vein or the superior mesenteric vein are often considered unresectable by surgeons worldwide. However, such tumors may not always be unresectable. The part of the vein and the percentage of the circumference of the vein that have been invaded must be thoroughly studied. This requires vast and highly specialized experience from both the surgeon and the radiologist, close collaboration, and advanced digital imaging technology. In many cases, removing the invaded part and replacing it with a graft (artificial graft, or coming from another vein in the patient’s body) is possible. Our team has implemented this method multiple times and has performed radical resections in tumors considered unresectable in Greece and abroad.
2. Unlike tumors with multiple distant metastases, tumors that spread and invade the portal vein, the superior mesenteric vein, and the pancreatic vein are considered “locally unresectable.” In such cases, neoadjuvant chemoradiation therapy is recommended. Neoadjuvant chemoradiation therapy significantly reduces the size of the tumor and downstages it, making it resectable and freeing up affected vessels.
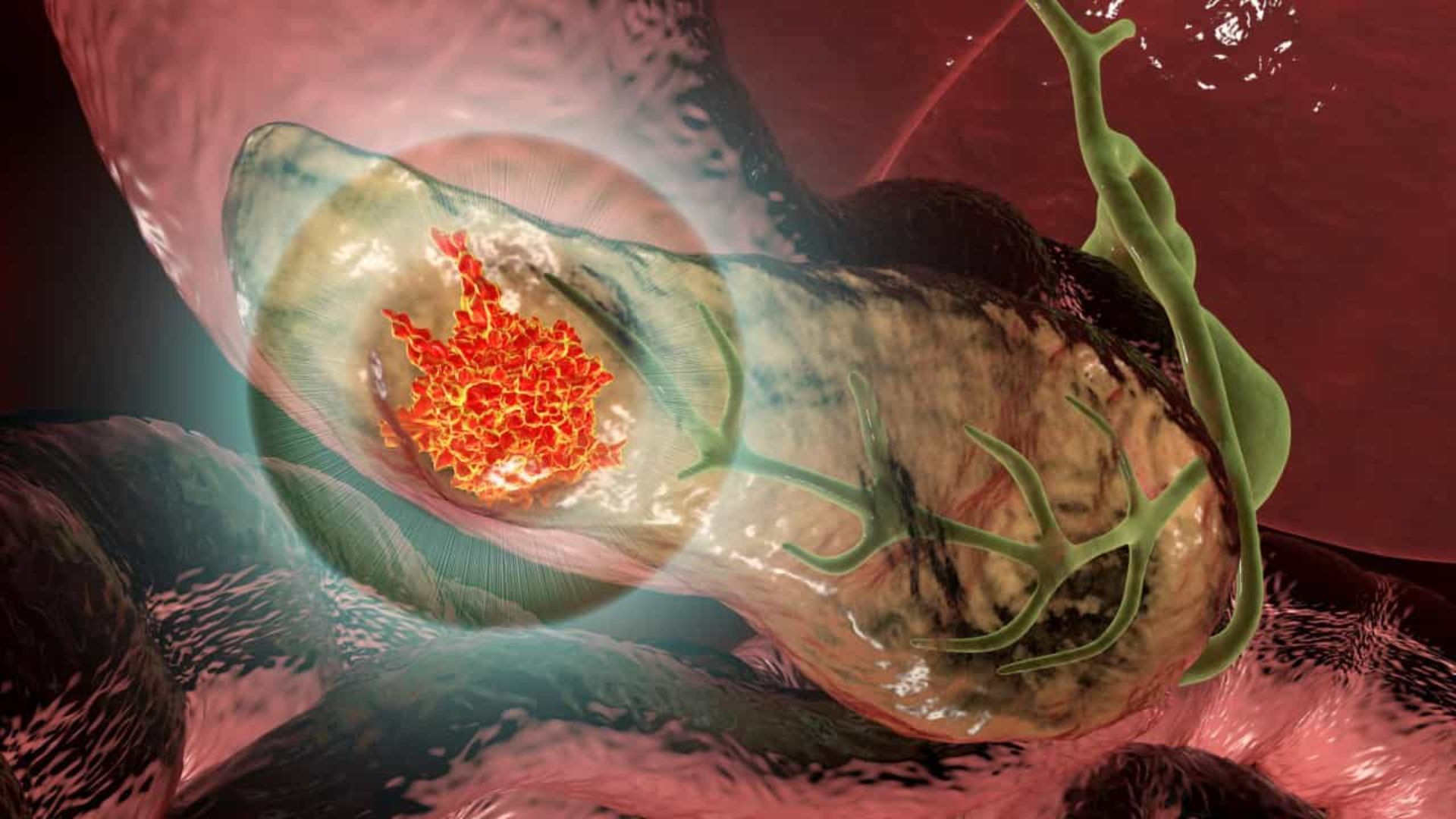
3. Pancreatectomy is a surgical procedure that involves the surgical resection of the parts of the pancreas that have been affected by the tumor, along with the surrounding fatty and lymphatic tissue. In this procedure, all arteries, and veins of the area (e.g., the portal vein, the superior mesenteric and splenic veins, the superior mesenteric and hepatic arteries, and the inferior vena cava, as shown in the image above) must be completely stripped. This allows us to perform extensive lymph node dissection (removal of more than 15-20 lymph nodes). Only in this way can a surgical procedure be considered radical and truly therapeutic. Any treatment that falls short of the above description is considered insufficient in terms of cancer treatment, and may lead to rapid tumor recurrence and metastases development.
4. Pancreatectomy with simultaneous resection of one or two coexisting liver metastases may be recommended to certain selected patients. It should be noted that this happens rarely and NEVER when multiple liver metastases are present. This method requires a surgeon with exceptional experience in both pancreatic and liver surgery. It is widely known that this method improves survival rates as opposed to approaches that favor leaving liver metastases untreated and treating them postoperatively with chemotherapy.
Generally, as in all other kinds of cancer affecting organs of the human body, radical pancreatectomy seems to be the only surgical procedure that provides an opportunity for comprehensive treatment. During pancreatectomy, we perform extended lymph node dissection and make coordinated efforts to convert unresectable tumors to resectable ones.