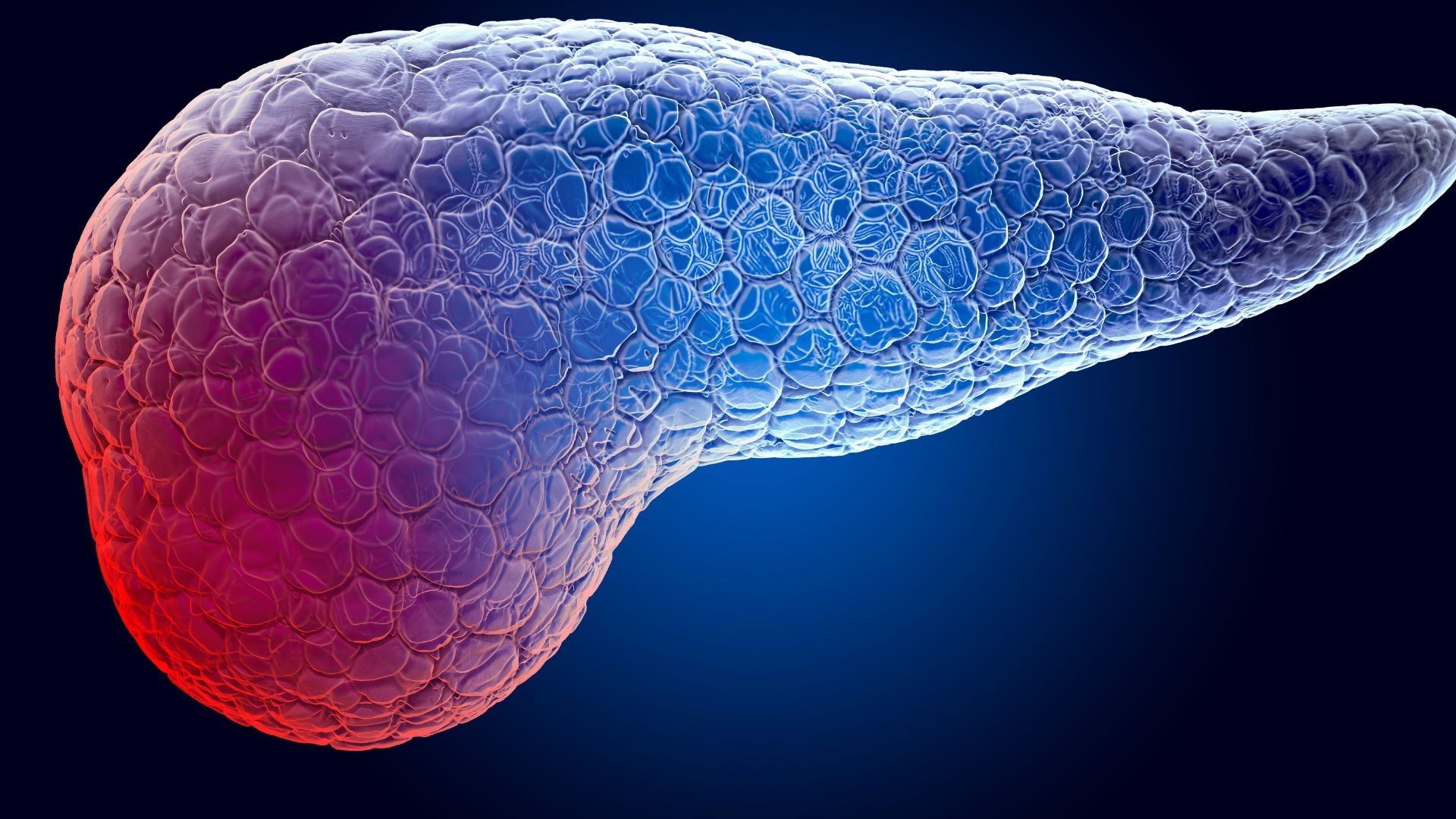
The Intraductal Papillary Mucinous Neoplasm (IPMN) of the pancreas is a condition that has been increasingly recorded over the past years due to the high frequency of ultrasound tests performed for various medical reasons. In IPMN, many small cysts are present in the pancreas and secrete large amounts of mucus. This mucus impedes the flow of pancreatic fluid and thus increases the chances of pancreatitis to occur. IPMN is significant for the two following reasons:
- It often leads to “unexplained” pancreatitis in patients without cholelithiasis, and
- It can progress into pancreatic cancer.
IPMN may be categorized in MD-IPMN (main pancreatic duct) and SB-IPMN (side branch) based on the areas of involvement. MD-IPMN is much more dangerous as it causes acute pancreatitis but also because it usually (80%) progresses into pancreatic cancer. On the other hand, SB-IPMN causes pancreatitis and progresses into cancer less often (10%). Magnetic resonance cholangiopancreatography (MRCP) is a special imaging test that helps doctors make an accurate diagnosis and differentiate between the two categories of IPMN. This test produces detailed images of the anatomy of the main pancreatic duct and its side branches.
Due to the increased likelihood of IPMN progressing into cancer, many conferences held over the past 15 years have established the criteria based on which patients may or may not undergo surgery. These criteria are referred to as “high-risk stigmata” or “worrisome features.” They are based on findings of the MRCP if the diameter of the main pancreatic duct is larger than 1cm, and mostly on findings of the endoscopic ultrasound and fine needle aspiration biopsy (EUS-FNA). Endoscopic ultrasound and fine needle aspiration is a test that can be performed safely by a few experienced and specialized gastroenterologists. If findings of the EUS-FNA indicate the presence of masses or septa within the cysts, or cells with dysmorphia, or if the CEA tumor marker of the cyst fluid is too high, the affected part of the pancreas shall be resected. If such findings are not the case, frequent monitoring by an experienced pancreatic surgeon is recommended. This way, the likelihood of progression is reduced, and unnecessary surgeries are avoided. Our team has extensive experience in this field, as the first relevant scientific publication was made by Mayo Clinic based on studies in which we participated. When surgery is deemed necessary, it is usually done laparoscopically.
Pancreatic cysts may be serous or mucinous. Serous cysts do not progress to cancer and shall be monitored for safety reasons unless they grow significantly and cause symptoms due to pressure. However, mucinous cysts often progress into cancer. A detailed analysis of their fluid should always be performed through EUS-FNA. When surgery is deemed necessary for mucinous cysts, it is done laparoscopically.