Παθήσεις Παγκρέατος (7)
Pseudocysts of the pancreas (PC) appear in 5% of patients after a severe acute pancreatitis episode (AP). The term “pancreatic pseudocyst” describes localized pancreatic fluid collections that occur 4-6 weeks after the onset of pancreatitis. Defining the term may be simple, but managing pancreatic pseudocysts is complex. Acute peripancreatic fluid collections developing after an episode of acute pancreatitis are often referred to as pseudocysts by gastroenterologists and surgeons. These fluid collections usually resolve without any special treatment. Localized fluid collections that usually contain solid tissue and necrotic debris and are nothing more than partially liquefied pancreatic necrosis are also erroneously referred to as pseudocysts.
Chronic alcohol abuse is a leading cause of chronic pancreatitis. Alcohol causes low-grade but ongoing inflammation (“irritation”) of the pancreas, which progresses and causes sclerosis of the pancreas, pancreatic duct abnormalities (abnormalities on the small tube that runs through the pancreas), and abnormal swelling of a part of the pancreas (resembling neoplasm). It also causes chronic pain in the upper and the middle part of the abdomen, diabetes mellitus that requires insulin, as well as inability to digest food correctly and fully. These symptoms lead to weight loss, increased feelings of weakness, and intake of multiple pain relievers that lead to addiction and dependence.
Diabetes mellitus and pancreatic cancer - Diabetes mellitus as an early sign of pancreatic cancer
Written by Super User Wednesday, 13 April 2022In medical literature, there has been an association between the onset of diabetes mellitus and pancreatic cancer since 1990. Indeed, it has been recorded that people who suddenly report increased blood sugar levels without having gained weight have eight (8) times higher risk of developing pancreatic cancer. This data illustrates a notable correlation between diabetes mellitus and pancreatic cancer. According to ongoing scientific studies, whose first results were presented at the annual meeting of the American Pancreatic Association in November 2013, there is a direct relationship between pancreatic cancer and new-onset diabetes mellitus. These findings came to confirm our observations. For years, our team has been noticing that two out of three patients (approximately 70%) with pancreatic cancer had developed type 2 diabetes mellitus one year before diagnosis. We had also noticed that this type of diabetes could not be attributed to any other cause, such as weight gain or a family history of diabetes. Patients who belonged to the above category were usually told to follow diabetes treatments without considering that diabetes could, in fact, be an early sign of pancreatic cancer. This relationship between diabetes mellitus and pancreatic cancer is due to Adrenomedullin, a protein produced by cancer cells of the pancreas well before other symptoms related to the tumor appear. Adrenomedullin inhibits the action of insulin, thus leading to the onset of diabetes mellitus with no further related symptoms.
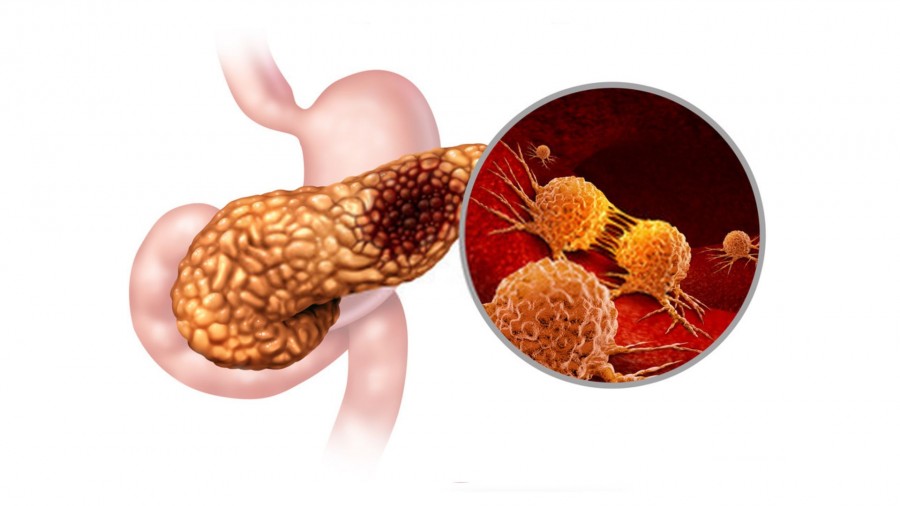
Cholelithiasis and alcohol abuse are two leading causes of acute pancreatitis. However, in rare cases, especially in younger patients, episodes of acute pancreatitis cannot be attributed to any of these two causes. In such cases, doctors usually recommend gallbladder removal surgery (cholecystectomy) or advise patients to see this episode as a single and isolated event. Although such an episode of acute pancreatitis may appear not to have an exact cause (unexplained), it may actually be the first sign of pancreatic cancer.
Acute pancreatitis is the sudden (not chronic) inflammation of the pancreas. The pancreas is situated deep in the abdomen. It lies behind the stomach and the large intestine, and is in close contact with major vessels. As its position indicates, its inflammation may affect the function of almost all organs in the abdomen. Acute pancreatitis is rather devious; it occurs suddenly and has no warning signs that could allow for a timely diagnosis. Preventing its progression is not easy. Often, patients are referred to general physicians or pathologists instead of highly specialized pancreatic surgeons. This is a common mistake as general physicians may not be familiar with current treatment methods that are very different from the methods employed 10 or even 5 years ago. Treatment methods are rapidly advancing with each passing day.
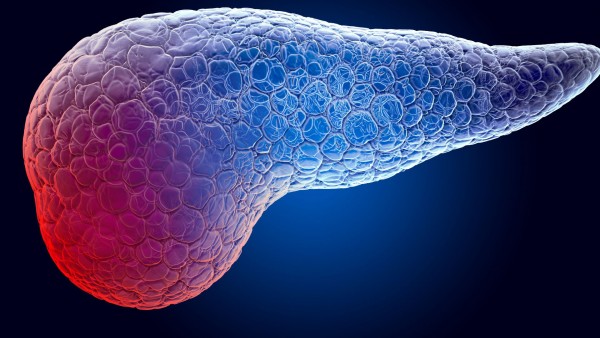
Neuroendocrine Tumors (NETs) are neoplasms (approximately 1% of the neoplasms of the pancreas) that tend to be more benign than regular pancreatic cancer. The biological behavior of Neuroendocrine Tumors (NETs) depends on their malignancy grade (e.g., Grades 1, 2, 3), which is defined by the Ki-67 index. CT- and MRI scans are and will be the basis of the diagnosis. Nowadays, gallium-68 somatostatin receptor scintigraphy is used for increased diagnostic accuracy when NETs need to be detected in other parts of the patient’s body. Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is used when a biopsy needs to be performed for NETs; however, it is not always necessary in patients with NETs initially considered resectable.
The Intraductal Papillary Mucinous Neoplasm (IPMN) of the pancreas is a condition that has been increasingly recorded over the past years due to the high frequency of ultrasound tests performed for various medical reasons. In IPMN, many small cysts are present in the pancreas and secrete large amounts of mucus. This mucus impedes the flow of pancreatic fluid and thus increases the chances of pancreatitis to occur. IPMN is significant for the two following reasons: